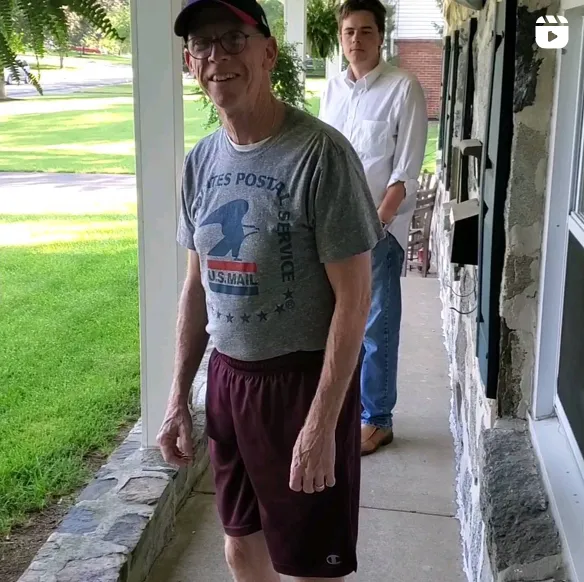
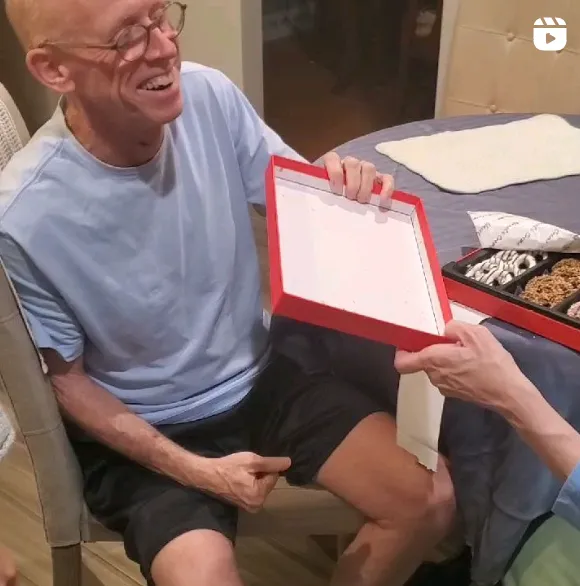
Managing a chronic disease is difficult. It’s a process of doctors’ visits, procedures, coping with flare-ups, and trying to get the best treatments to go back into remission. Unfortunately, some chronic diseases have no cure.
Paroxysmal nocturnal hemoglobinuria, also known as PNH, is a rare disease that is still without a cure. At least 400-500 cases are diagnosed annually in the country. Despite the lack of a cure, physicians and researchers continue to seek ways to defeat chronic diseases like PNH. They aspire to improve treatments for patients and improve their quality of life.
Below is everything you need to know about PNH, and what is currently being done for the disease today.
What is PNH?
Paroxysmal Nocturnal Hemoglobinuria is a rare blood disease. The condition causes red blood cells to break apart or disintegrate, which is called hemolysis. Due to the lack of a specific protective protein, known as GPI-anchored proteins that coat and defend the surface of the red blood cells, the cells become weak and break to pieces, releasing the hemoglobin inside. It’s this release of hemoglobin that triggers a number of the symptoms of PNH. PNH can cause blood clots and impaired bone marrow function. The disease is associated with aplastic anemia.
The name references passing dark-colored urine, particularly at night. Though while some patients do have dark-colored urine because of the hemoglobin, a large percentage of those who have PNH do not.
PNH is seen as a disease stemming from bone marrow failure. When blood cells produced by bone marrow are damaged or defective, or if the marrow is unable to provide enough of them, it’s referred to as a bone marrow failure. This blood disease is also considered life-threatening.
Advances in PNH Treatment and Research
Near the end of 2018, PNH gained greater awareness when the Food and Drug Administration officially approved the use of a new drug, ravulizumab-cwvz, or Ultomiris, as a treatment for the disease.
The drug is part of what is called complement therapeutics: it addresses the lack of complement-regulating protein cells that keep healthy cells from disintegrating. The medication works on the complement process to manage the symptoms of PNH and save lives. However, the drug can have side effects, including increased risk of meningococcal infections and sepsis.
Another treatment that is currently in development and has received attention is APL-2, or pegcetacoplan. It was fast-tracked as a novel treatment that could be used against PNH. APL-2 is designed to inhibit the complement cascade, and it even can potentially aid in the treatment of other complement-mediated diseases.
Danicopan is another treatment that has been given a Breakthrough Therapy designation by the FDA. Researchers have shown promise in its ability to improve anemia as measured by hemoglobin. Furthermore, trial subjects saw a reduction in blood transfusions and an increase in the hemoglobin of patients who completed the treatment for 24 weeks.
While there may still be no cure on the horizon for PNH, the breakthrough drugs that are now being fast-tracked or put into priority by the FDA show that there are big leaps and advancements in research towards the disease. With better treatments and improved drugs, there is hope that the quality of life of people afflicted with PNH may improve.
PicnicHealth also supports research on PNH by structuring real-world evidence datasets from anonymized medical records of real people living with PNH in the real world. Visit PicnicHealth.com to sign up for a free PicnicHealth account and contribute to research if you have PNH.