One evening last month, three members of the rare disease community from Malaysia, the U.S. and the U.K. came together for a discussion about mental health. Sivasangaran Kumaran is the father of Swathi, who has Pompe disease. Frank Rivera is President of Sarcoidosis of Long Island, as well as the Founder of Stronger Than Sarcoidosis. David Ross, who organized the discussion, hosts international Zoom meetings for other men who, like himself, have been impacted by rare disease. According to research, men are less likely than women to seek mental health treatment, and some men have a harder time forming social connections. David’s meetings, called the Rare Disease Awareness Men’s Group, seek to acknowledge and address these two issues for men in the rare disease community.
Sivasangaran, Frank and David spoke about the impact rare disease has had on their mental health, family dynamics and their drive to build community and raise awareness. Their conversation is below.
Finding Community Post-Diagnosis
Sivasangaran: It definitely started with real people in my real life. Both my family and my in-laws were really great. My colleagues back at the office said, “Drop everything that you're doing in your office, go, and we’ll manage it for you.”
The first thing that we all do, when we don't know anything, we'll search online. I found a local NGO (non-governmental organization) who actually was championing Pompe disease. I met three other parents with kids at different ages but similar stages. I had millions of questions and they had plenty of answers, but, sooner or later I realized that not every child with Pompe disease is the same.
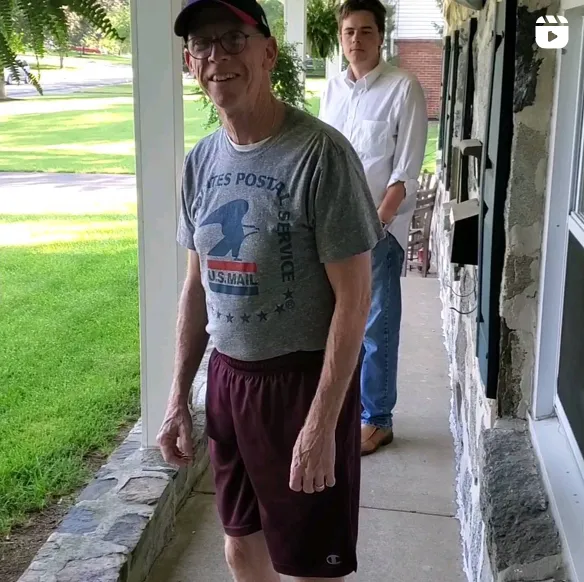
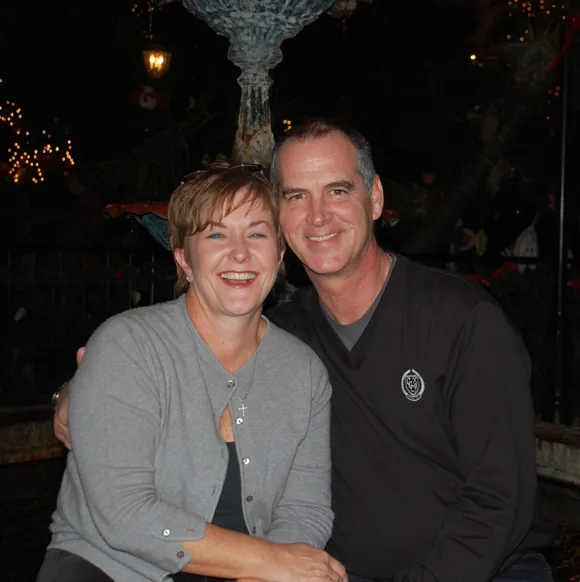
Frank: My immediate family has been great. My wife married me knowing I had sarcoidosis, and she’s been there every step — she’s as well known as I am in the sarcoidosis community. My daughter, she’s there for me. Since my disease is an “invisible” disease, a lot of people outside the immediate family don’t understand it. People have gotten upset with me if I couldn’t attend family gatherings because I’m sick in bed. That can make it hard. I’ve lost friends but I’ve also gained a whole new rare disease community.
Back when I was diagnosed, there was a national organization, the Foundation for Sarcoidosis Research, but at the time they were more into research than working with patients, so I really didn’t have anyone to talk to at first. That’s why I started an organization myself: Sarcoidosis of Long Island. Doing that really helped me out and gave me a reason to fight and to help others.
David: Something I’ve realized since the early days of diagnosis was how many amazing women there were talking about the condition, but there weren't so many men. I also learned that quite a few men in my own rare disease community at that point were suffering with mental health, but weren’t able to seek support and speak about what they were going through. So last year I started up international Zoom calls for rare disease patients and caregivers, with the idea of bringing men together to talk about what they're going through, sharing their experiences in a safe space and building some sort of regular support.
Navigating Mental Health
Frank: I’m Hispanic; we don’t really, don’t believe in talking about their mental health [laughs]. Especially males — they’re supposed to be the Alpha, just let it roll off — and that’s how I grew up. My father was sick all his life, yet he wouldn’t talk about it. When I first got diagnosed, that’s what I thought, “Alright, deal with it.” Plus, I was still able to work. Then, in 2014, I went on disability and that was tough.
It's definitely okay if you're a guy and asking to go see a counselor. You should not be embarrassed. When you don't ask for help and you’re just keeping it in, all you're doing is hurting yourself.
I see a counselor and have for a long time now. It took me awhile, but I realized that it was okay to be emotional. It's okay to have bad days and it's okay to have good days and it's okay to talk about it. That's where I'm at.
David: The process starts with seeking support. But also, it’s something you have to learn through experience. You’re starting at the beginning working your way through it. Because it’s rare, you’re still trying to make sense of it all. And as you're learning the most about your condition, you're learning as well as treating and maintaining your mental health.
Something that’s always stuck with me – in my early days of diagnosis, I went to an event in London at the Houses of Parliament and met someone from another rare disease community, the first person I spoke to from the community, and he said, “If you can accept that you have a rare disease, that’s half the battle.” That’s always stuck with me — acceptance — everything around that is quite important to remember.
Making Mental Health Important for Everyone Affected by Rare Diseases
Sivasangaran: In certain ways, the rare disease community’s voice is small by nature. We are still fighting for rare disease to be acknowledged and to create awareness. It's best when we can partner with the people who are championing mental health as a primary concern and tag along with them and spread messages together. Us as part of them, rather than me trying to include them as part of us.
For example, we have a local movement that does mental health awareness and fights for the mental health benefits from the government. We partnered with them and made them aware that, “Hey, this community exists and we face the same challenge — can we partner together and move along to support your cause?”
Frank: Like Siva, we’ve been turning our virtual groups into partnerships with Mental Health America (MHA) or National Alliance on Mental Illness (NAMI). They come to our meetings and we talk about mental health as much as the physical effects of the disease now. But it’s also to help educate the MHA and their staff that yes, mental health is all encompassing, but there are different aspects with a rare disease patient. Another obstacle for some rare disease patients sometimes is that when you go to a counselor, they don’t understand you because they don’t understand the disease.
If you work together you meet more people and people will realize we have different diseases and symptoms, but there’s a lot of similarities, especially with mental health challenges. Once people realize that, we are stronger.
Sivasangaran: If I may add — though we’re adults addressing the topic, I'm sure children's mental health is equally important as well. It'll be good if we can also increase the space for children. To ask my son, “How is it having a sister with a rare disease?” How does it feel when he sees his parents are moving around with his sister to the hospital, after another hospital, and then he has to be left alone with his grandparents?
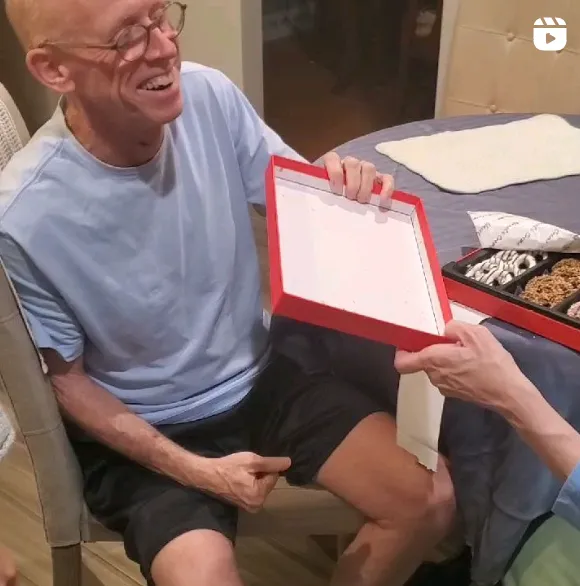
Frank: We also sometimes forget about the caregivers and their mental health. They may not physically have the disease, but they’re living with it too.
I have family members who see a counselor to help manage the effects of this disease. My wife has to work because I can’t. She has to get groceries after working a full day because I can’t sometimes. They can be forgotten about a lot of times.
David: My daughter is 15 but she lost her grandmother, my mother, to a rare disease and my nephew last year, and her mental health has been impacted by that. My side of the family isn’t really there anymore. The children need their voice for their mental health as well as the caregivers, they need to be in focus too. We all do.